Nearly 3 percent of the world’s population has some form of psoriasis—that’s over 125 million people. Of those, an estimated 7.5 million are Americans, according to the National Psoriasis Foundation (NPF), making it the most common autoimmune disease in the country.
Although this skin disease is prevalent, many people are still unaware of its impact. Unfortunately, there are many misconceptions about the disease; for example, that it is contagious.
What is Psoriasis?
Psoriasis is a chronic autoimmune disease that causes skin cells to multiply up to 10 times faster than normal. This makes the skin build up into bumpy red patches covered with white scales that can grow anywhere, but typically appear on the scalp, elbows, knees, and lower back. Psoriasis is not contagious nor is it caused or worsened by poor personal hygiene. Psoriasis may be inherited and can range from a very mild, hardly noticeable rash to a severe eruption that covers large areas of the body. Affiliated Dermatology’s Dr. Andrew Newman shares some facts about psoriasis:
“Although psoriasis is typically thought to be a condition that only affects the skin, it affects the ENTIRE body. In fact, joint disease, heart disease, and depression are common features in psoriasis. It’s caused by many factors including genetic predisposition, certain medications, and some infections such as strep throat. People with psoriasis most often are regularly taken care of by a dermatologist.”
In some patients, psoriasis causes nail changes and joint pain (psoriatic arthritis). The first episode usually strikes between the ages of 15 and 35. This chronic condition will then cycle through flare-ups and remissions throughout the rest of the patient’s life.
Types of Psoriasis
The most common form of the disease, plaque psoriasis, appears as raised, red patches covered with an accumulation of white dead skin cells. Other areas affected by the different types of psoriasis include the face, skin folds, hands, feet, genitals, and nails.
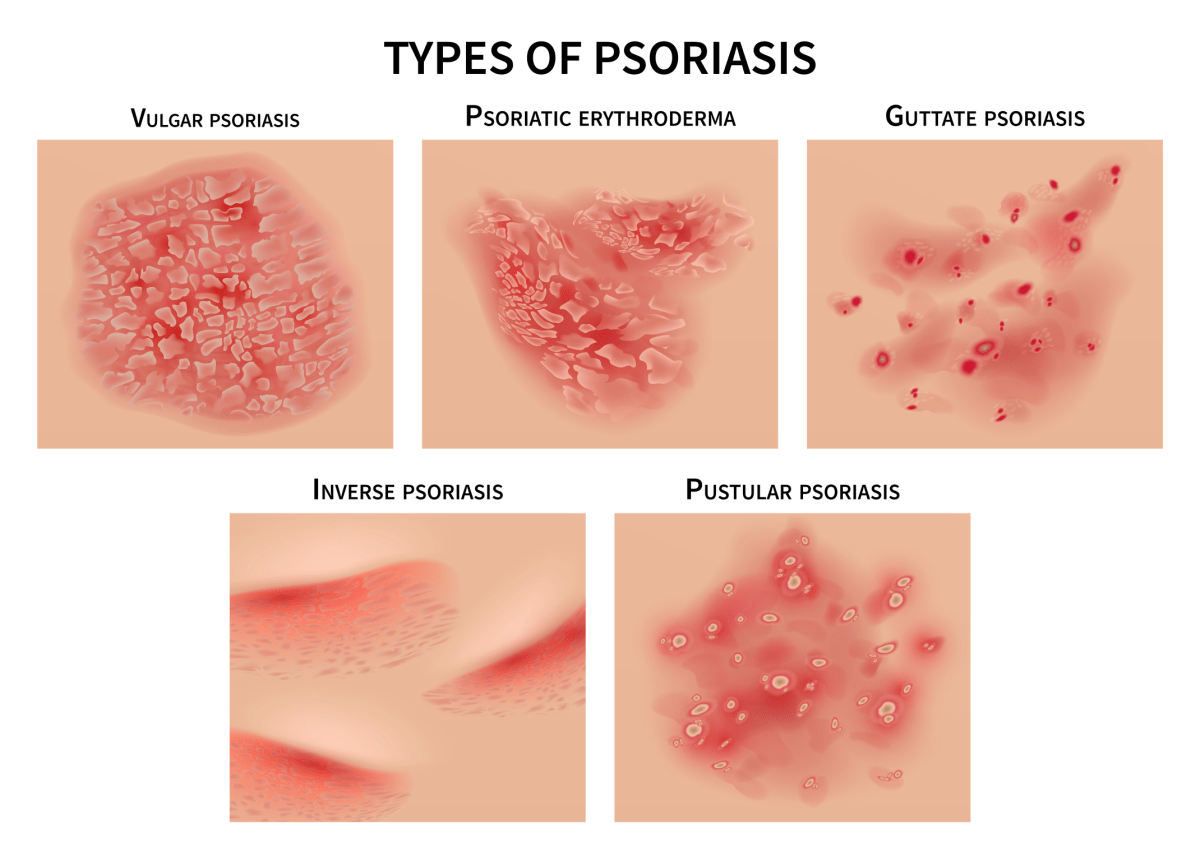
- Pustular psoriasis causes red and scaly skin with tiny pustules on the palms of the hands and soles of the feet.
- Guttate psoriasis often starts in childhood or young adulthood, causes small, red spots, mainly on the torso and limbs. Triggers may be respiratory infections, strep throat, tonsillitis, stress, injury to the skin, and taking antimalarial and beta-blocker medications.
- Inverse psoriasis makes bright red, shiny lesions that appear in skin folds, such as the armpits, groin, and under the breasts.
- Erythrodermic psoriasis causes fiery redness of the skin and shedding of scales in sheets. It’s triggered by severe sunburn, infections, certain medications, and stopping some kinds of psoriasis treatment. It needs to be treated immediately because it can lead to severe illness.
- Scalp psoriasis can cause dandruff-like itching and flaking. Psoriasis happens when the immune system triggers too many skin cells to grow on various parts of the body. That can include your scalp. People with psoriasis may be more likely to get dandruff, but psoriasis is not dandruff.
What causes Psoriasis?
Although psoriasis appears on the skin, it is an immune system disease that is not caused or worsened by poor personal hygiene. People with the disease have a genetic tendency to develop it. There are certain things that can trigger flare-ups including skin injury, stress, hormonal changes, infection, and medications. Most people with the disease experience cycles of clear skin and outbreaks. Dr. Dustin Mullens of Affiliated Dermatology spoke on how Psoriasis starts:
“The nervous system and stress affect a multitude of skin conditions in humans. There are many types of cells in the skin affected such as immune cells and endothelial cells, both can be regulated by neuropeptides and neurotransmitters, which are chemicals released by the skin’s nerve endings. Stress can result in the skin’s nerve endings releasing an increased level of these chemicals and when this occurs, it can lead to inflammation of the skin. This is why people often experience a flare-up of their inflammatory skin conditions such as psoriasis during times of stress.”Things that can trigger an outbreak of psoriasis include:
- Cuts, scrapes, or surgery
- Emotional stress
- Strep infections
- Medications, including
- Blood pressure medications (like beta-blockers)
- Hydroxychloroquine, antimalarial medication
Symptoms of Psoriasis
The truth is that there are many people with psoriasis who don’t even know they have it! Skin rashes are not uncommon so dermatologists need to rule out a list of other possible causes like an allergy to food/medication and viruses. Careful visual inspection is needed for diagnosing psoriasis, but sometimes there is a need for a skin biopsy.
Is infection a possibility? Infections are actually quite rare due to the fact that psoriasis itself is due to an overactive immune system. That being said, repeated scratching and excoriation can disrupt the skin barrier and facilitate bacterial invasion and is thus strongly discouraged. All patients with psoriasis should be seen at the very least annually by a dermatologist and when treatment and medications are ineffective at controlling disease severity and flares. Patients requiring systemic treatment should be seen every 3 months for check-ups while on these more sophisticated/complex medications.
How to Treat Psoriasis?
There’s currently no cure for this chronic autoimmune condition, but caring for psoriasis can slow down the growth of skin cells and relieve pain, itching, and discomfort. Treatment of psoriasis depends on a patient’s overall health, presence of joint pain, and severity of skin involvement. When asked about treatment for psoriasis, Dr. Newman shares,
“The type of treatment used depends on the total body surface area involved and severity, etc. In mild psoriasis, I think natural medicines work well. Some people find benefit from taking the natural anti-inflammatories quercetin and curcumin. Additionally, they may find that applying aloe vera gel to the skin does wonders. Lastly, sunlight also helps with mild psoriasis. That’s right, the UV rays of the sun decrease the skin inflammation in psoriasis! In fact, this explains why my colleagues and I see less psoriasis where we practice in the sun-rich Phoenix, Arizona, compared to areas like the midwest.”
In mild cases, topical corticosteroids and medications are prescribed. Psoriasis is not curable, but it is controllable. No single approach works for everyone. Therapy is individually tailored and based on your health, goals, and a careful assessment of potential risks and benefits of treatment. Treatments can be divided into four main types:
- Topical treatments
- Light therapy
- Systemic medications
- Biologics
Dr. Newman goes on to say, “For more serious psoriasis, it will be almost impossible to successfully manage the disease without sophisticated prescription medicines. Usually, this will entail potent topical corticosteroids and/or certain oral or injectable medicines that help regulate the body’s immune system (which has gone haywire in psoriasis). Importantly, if you have psoriasis (mild or severe), you should discuss the use of both natural and prescription medicines with your primary care doctor and your dermatologist.”
Find Relief for Psoriasis
The best treatment varies by individual, taking into consideration the type of psoriasis you have, where it is on your body and the possible side effects of medications. Another AffDerm dermatologist, Dr. Mitchell Manway, gave us some extra tips on what to do when you have psoriasis.
Moisturizers: which kind are the best? “In general, the thicker or greasier the moisturizer, the better. Creams and ointments that come in a tub or jar are more effective at restoring the skin barrier than lotions or products that come in pump-dispensers. Products containing petrolatum or ceramides can be particularly effective or preferred,” says Dr. Manway.
Scale softening products? What ingredients work best? Dr. Manway advises, “Products that contain lactic acid (Amlactin/Lac Hydrin), salicylic acid (Salex), or urea are more effective at removing scale and improving skin texture.”
Cold showers/cold packs or warm baths/heating pads? According to Dr. Manway, “Ice-packs and heat may be effective at treating symptoms of itch by distracting nerve receptors, but I would avoid exposure to showers or bathing as this may promote further water-loss and drying of the skin.”
Stress relief options like meditation, acupuncture, etc? “Studies directly involving acupuncture and treatment of psoriasis are still inconclusive, with some proposing benefit and others with no significant results. However, anything that can promote stress relief may be helpful at preventing and controlling flare-ups as stress can be a major contributor for worsening of the disease,” said Dr. Manway
Exercise? “Daily or weekly exercise can stimulate and regulate the immune system and decrease stress levels, and thus is an important part of disease management.”
Over-the-counter remedies like calamine lotion? “In my experience calamine lotion is not very effective at reducing itch or pain. Topical preparations that contain pramoxine (Sarna Sensitive) or menthol (Sarna) are preferred. Surprisingly, brief periods of exposure to sunlight and UV rays can also benefit psoriasis, but limited exposure should be stressed due to the increased risk of skin cancer associated with chronic UVA and UVB damage,” said Dr. Manway.
Prescription medications? Dr. Manway agrees, “Rx medications are by far the most effective topical treatment approach available and help to decrease inflammation at the site of disease. Potent topical steroids such as clobetasol or betamethasone are the most common medications prescribed, but other mechanisms such as vitamin D analogues and calcineurin inhibitors can provide significant and adjunct benefits towards the reduction of psoriatic plaques with less risk of long-term local side-effects. When local disease can not be maintained on topical medications or development of psoriatic arthritis is present, systemic oral medications or biologic therapy/injections are necessary.”
When should you see your dermatologist for psoriasis? Look out for any suspicious changes such as lesions that show signs of persistent flaking, scaling, roughness, redness, scabbing, bleeding, or otherwise non-healing areas. These symptoms are uncomfortable and could be an indication of something more serious.
If you have psoriasis or think you do, contact your dermatologist and let them help you find a treatment plan that works best for you.






